
At the beginning of prenatal care, your doctor or midwife will likely run a series of blood tests. These should include:
- Complete Blood Count (CBC) to determine the quality and content of your blood.
- Blood Typing to determine your blood type and Rh factor (positive or negative).
- Coombs Test (or Antibody Screen) to determine if antibodies that are potentially harmful to the fetus are present in the mother’s blood.
The test results will influence your practitioner’s recommendation for administering RhoGAM.
What is a Rh Factor?
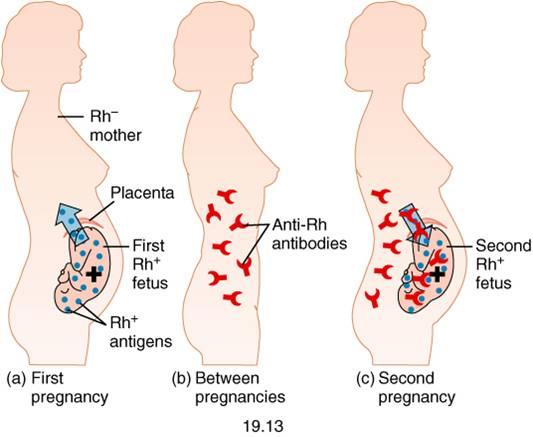
Around 83 percent of woman carry the antigen know as Rh factor in their blood. These women are Rh positive. The remaining 17 percent do not carry this antigen, making them Rh negative. For example, a woman with the “A” blood type carrying the Rh factor is “A+”, without the Rh factor she is “A-“. If the mother is Rh negative, most practitioners assume her baby is Rh positive. If Rh negative maternal and Rh positive fetal blood mix, the mother will develop antibodies that can cause hematolytic disease of the fetus and newborn (HDFN) in future pregnancies.
The Circulatory System
During a normal pregnancy, a mother’s bloodstream never mixes with that of her baby’s. Her blood flows to her uterus and passes oxygen, nutrients, and antibodies through the placenta to her baby’s blood. This blood then travels up the umbilical vein, through the baby’s circulatory system, and back to the placenta through the umbilical arteries. The blood travelling through the umbilical arteries carries waste products and carbon dioxide. Maternal and fetal blood may mix in the event of trauma, abortion, miscarriage, or ectopic pregnancy. Mixing can also occur during labor, at the separation of the placenta or during a C-section.
What is RhoGAM?
RhoGAM (the most popular anti-D brand in the USA) is an injection designed to prevent the mother’s body from developing antibodies against Rh positive blood. It first entered the market in 1968 and is derived from human blood plasma. It is believed to have decreased the cases of Rh-sensitization and HDFN. The current standard of care both in the United States and Europe is to administer RhoGAM (or another anti-D variation) during the 28th week of pregnancy or within 72 hours of a sensitizing event (such as abdominal trauma) before the 28th week. RhoGAM is administered once again within 72 hours of delivery if the newborn is Rh+.
Other Considerations
Things to consider about RhoGAM include:
- Rh factor of the baby’s father
- Likelihood of future children
- Personal or religious convictions about vaccinations and blood products
A mother might consider declining RohGAM for the following reasons:
- If both the baby’s mother and father are Rh negative, the baby will be Rh negative, making RhoGAM unnecessary.
- Since Rh-sensitization takes time to occur, the current fetus is less affected than future children, therefore, the need for RhoGAM decreases if future pregnancies are unlikely.
- Like all vaccines, RhoGAM carries risks (anaphylactic shock, transmission of disease, etc.) as it contains human blood product and other chemicals common to vaccines.
In the past, less was understood about Rh factors, compatibility, and vaccines. We are fortunate to live in a time when “informed consent” can truly be informed.
Want new articles before they get published?
Subscribe to our Awesome Newsletter.
